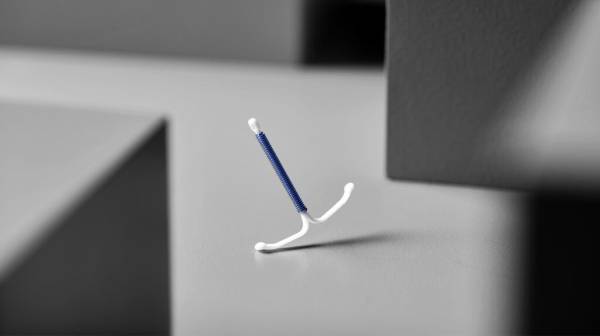
Share on PinterestIntrauterine devices (IUDs) can increase breast cancer risk by a similar margin compared to contraceptive pills, a recent study found. Image credit: Martí Sans/Stocksy.
- Intrauterine devices (IUDs) are the third most common form of modern birth control used around the world.
- There are two types of IUDs — copper IUDs that do not release any hormones and hormonal IUDs that release a synthetic form of the hormone progesterone.
- Previous studies show that hormonal IUDs may be associated with an increased risk of developing breast cancer.
- Researchers from the Danish Cancer Society Research Center have found an association between levonorgestrel-releasing intrauterine systems (LNG-IUSs) and increased breast cancer risk in females aged 15 to 49, compared to those who did not use hormonal IUDs.
As of 2021, about 874 million cisgender women around the world were using some type of modern contraceptive method, which include condoms, birth control pills, and intrauterine devices (IUDs).
IUDs are the third most common form of birth control globally, used by about 17% of women.
There are two types of IUDs currently available — copper IUDs that do not contain hormones and hormonal IUDs that release a synthetic version of the hormone progesterone that is called progestin.
Some hormonal IUDs — such as Mirena and Kyleena — use a specific type of synthetic progesterone called levonorgestrel.
Previous studies show that hormonal IUDs may be associated with an increased risk of developing breast cancer.
Now researchers from the Danish Cancer Society Research Center in Copenhagen, Denmark add to this body of research with a new study that has found an association between levonorgestrel-releasing intrauterine systems (LNG-IUSs) and increased breast cancer risk in females aged 15 to 49, compared to those who did not use hormonal IUDs.
The study was recently published in the journal JAMA.
How levonorgestrel-releasing IUDs can affect breast cancer risk
For this study, researchers analyzed data from more than 78,000 Danish first-time users of LNG-IUSs between the ages of 15 and 49 between the years 2000 to 2019, who were matched up to the same amount of nonusers of hormonal IUDs.
“We wanted to explore the long-term health effects of particularly hormonal IUDs, as they are becoming more widely used,” Lina Steinrud Mørch, MSc, PhD, senior researcher and leader of the Cancer and Medicine team at the Danish Cancer Society Research Center in Copenhagen, Denmark, and corresponding author of this study explained to Medical News Today.
She noted that:
“Understanding any potential links to breast cancer is crucial for informed choices about reproductive health. There has been concern about the impact of progestins on breast cancer risk, especially since we know that hormone replacement therapies during menopause can increase this risk. The hormone IUD is a progestin-only product.”
“A levonorgestrel-releasing IUD is a small device inserted into the uterus that releases a hormone called levonorgestrel,” Mørch continued. “This hormone prevents pregnancy by thickening cervical mucus to block sperm and thinning the uterine lining to prevent a fertilized egg from implanting. Today we have a ‘high dose’ IUD and low dose IUDs. This study assessed the high dose IUD mainly.”
IUD use linked to 14 breast cancer cases per every 10,000 women
Study participants were followed from the year they started until December 2022, equaling an average of 6.8 years. During that time, 1,617 participants were diagnosed with breast cancer — 720 were hormonal IUD users and 897 were not.
Upon analysis, Mørch and her team found hormonal IUD use was associated with an “excess risk” of 14 breast cancer diagnoses per every 10,000 women.
“This figure helps quantify the potential impact of hormonal IUDs on breast cancer risk,” Mørch explained. “It provides a clearer picture for women and healthcare providers about the risks involved, allowing for better-informed decisions regarding contraceptive options.“’
“The mentioned result can also be communicated in another way: for every 714 women using their first ‘high dose’ hormone IUD for 5 years, one woman will develop breast cancer due to the hormone IUD,” she added.
“It is important to remember that it is healthy women using this product for birth control, therefore the tolerance for severe side effects is low,” Mørch continued. “However, some women use the hormone IUD for other reasons than contraception. An example is treatment of pain in relation to menstruation. The benefits of the hormone IUD, can for some women outweigh the risk.”
“The ‘high dose’ hormone IUD is working — not only locally — but also systemically in the body. Therefore, the high dose hormone IUD is not ‘risk-free.’ Women in their 30s and 40s should be aware of the potential increased breast cancer risk associated with the ‘high-dose’ hormone IUD, and it’s important to include this knowledge in the discussion with healthcare providers of benefits and risks when considering contraceptive options.”
– Lina Steinrud Mørch, MSc, PhD
Breast cancer risk: How do IUDs compare to contraceptive pills?
After reviewing this research, Nora J. Doty, MD, a complex family planning specialist in the Department of Obstetrics and Gynecology at Hackensack Meridian Jersey Shore University Medical Center in New Jersey, told MNT that while this study shows an association between hormonal IUD use and breast cancer, but the actual increase in risk is very small.
“This risk found in this study is similar to other studies that have found a slightly increased risk of breast cancer diagnoses in current or recent combined oral contraceptive pill users,” Doty explained.
“However,“ she cautioned, “it is important to note that hormonal contraception also decreases the risk of other cancers, like endometrial and ovarian cancer. Importantly, hormonal contraception is only associated with diagnosis of breast cancer and not an increased risk of mortality from breast cancer.”
“All contraceptive methods have risks and benefits,” Doty continued. “The balance of these risks and benefits differs for each individual based on their family planning goals and individual health history.“
She advised that that: “Hormonal IUDs remain a really great way to prevent pregnancy and manage menstrual-related conditions. Everyone should discuss their individual health goals with their trusted reproductive health provider to find a contraceptive method that works best for you. For all women, it is also important to understand your individual risk of breast cancer and follow breast cancer screening recommendations from your healthcare provider.”
Breast cancer risk: Other variables need to be accounted for
MNT also spoke with Parvin Peddi, MD, a medical oncologist and director of Breast Medical Oncology for the Margie Petersen Breast Center at Providence Saint John’s Health Center and Associate Professor of Medical Oncology at Saint John’s Cancer Institute in Santa Monica, CA, about this study.
“This study showed a small increased risk of breast cancer using a Danish population database,” Peddi said.
However, she cautioned that: “It was not a randomized study and there may be confounding variables that were not controlled for. Furthermore, although a trend was seen, it was not significant for association of longer duration of using a hormonal based IUD and breast cancer risk. This may mean, the population was too small to determine this trend for sure or that the relationship does not exist.”
“In general, we have enough data from birth control pills that this is consistent with to say it is probably true that extra hormones, whether in birth control or in IUD, increase the risk of breast cancer,” Peddi noted.
“However, this increased risk is small. Therefore, a discussion needs to happen with [t]he) patient’s [gynecologist]/primary care doctor at time of initiation that puts this in context with their other risk factors — family history, any known genetic mutations, any prior history of breast findings — and need for a form of contraceptive,“ she continued.
“With careful monitoring, [the] majority of women are safe to use these IUDs for contraceptive methods. Further studies that corroborate these findings in other patient populations would be helpful,” said Peddi.





